As scientists edge closer to developing a universal antivenom capable of neutralizing venoms from multiple snake species, the potential for a revolution in the treatment of the estimated 5.4 million annual snakebites worldwide is on the horizon. However, the question remains whether such a broad-spectrum solution can effectively reach and save lives in remote, resource-limited areas where snakebites are most fatal.
The Global Burden of Snakebites

Snakebites pose a significant global health issue, disproportionately affecting rural populations in sub-Saharan Africa, South Asia, and Southeast Asia. These regions often suffer from limited access to medical care, exacerbating the problem. The World Health Organization estimates that over 100,000 deaths occur annually due to snakebites, highlighting the urgency of this issue. The current treatments often fail due to their specificity, requiring the exact identification of the snake species, which is often impossible under field conditions.
Socioeconomic factors such as poverty and lack of infrastructure in high-risk regions further exacerbate the mortality rates. The inability to access or afford antivenom treatments, coupled with a lack of education about snakebite prevention and first aid, contribute to the high fatality rates in these regions.
Limitations of Traditional Antivenoms

Existing antivenoms are species-specific, meaning they can only neutralize the venom of the snake species they were designed for. This necessitates the precise identification of the biting snake, which is often impossible in field conditions. Moreover, the production of these antivenoms relies on animal-derived antibodies, which can cause severe allergic reactions in up to 10% of patients, adding another layer of complexity to the treatment process.
Distribution barriers also pose significant challenges. The high costs associated with antivenom production and their short shelf lives often prevent effective delivery to endemic areas. These factors combined make the development of a universal antivenom a critical need in global health.
Another limitation of traditional antivenoms is the complex and time-consuming production process. It involves injecting a horse or sheep with small amounts of venom, then collecting the resulting antibodies from the animal’s blood. This process can take up to six months, making it difficult to respond quickly to sudden increases in demand. Additionally, the use of animal-derived antibodies raises ethical concerns about animal welfare, further complicating the production process.
Furthermore, the effectiveness of traditional antivenoms can be compromised by the evolution of snake venoms. Snakes continually evolve their venom composition to overcome the resistance of their prey, which can render existing antivenoms ineffective. This constant need for updates adds to the cost and complexity of traditional antivenom production.
Breakthroughs in Universal Antivenom Research

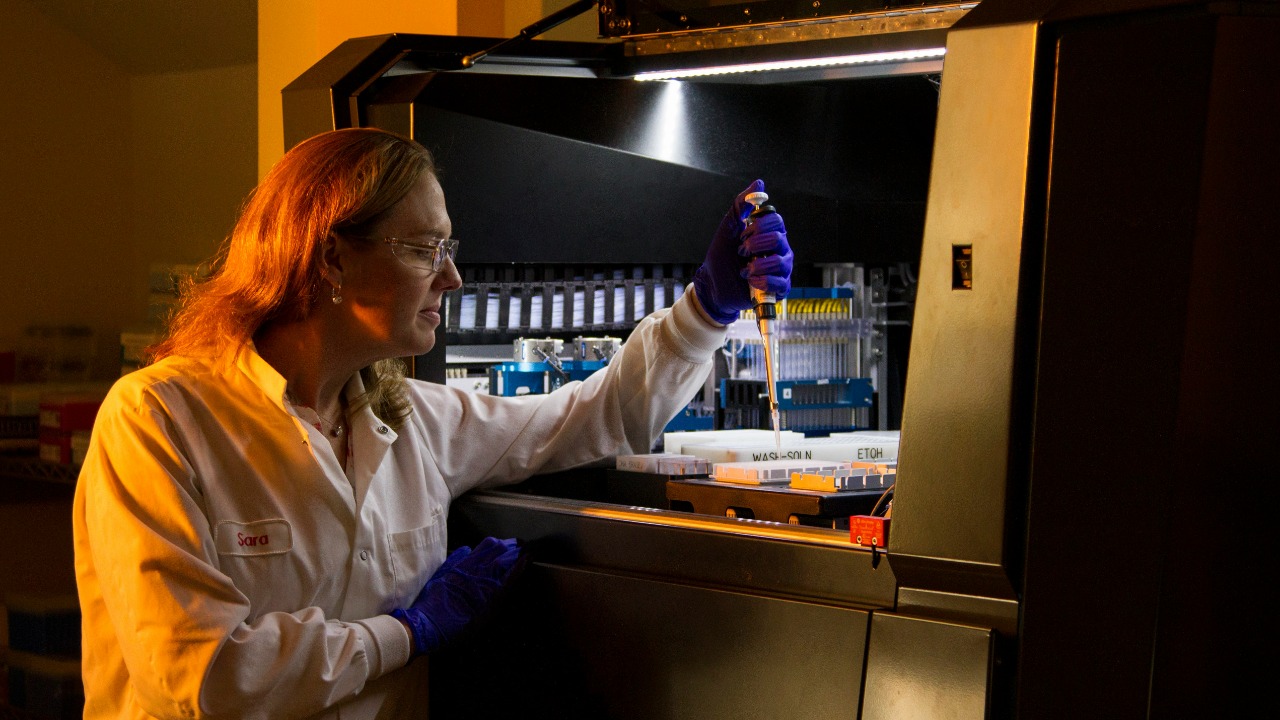
Scientific advancements are paving the way towards a universal antivenom. Approaches such as synthetic antibody engineering and toxin-neutralizing peptides aim to create a one-size-fits-all solution. Ongoing trials and preclinical successes have shown promising results, with lab tests demonstrating efficacy against venoms from major genera like vipers and elapids.
Leading researchers and institutions worldwide are driving this innovation, emphasizing the importance of collaborative efforts across international labs. The development of a universal antivenom could mark a significant turning point in the treatment of snakebites, potentially saving thousands of lives each year.
One of the most promising breakthroughs in universal antivenom research is the use of nanobodies, which are small, stable antibody fragments derived from camelids. These nanobodies can be engineered to bind to a wide range of toxins, making them a potential candidate for a universal antivenom. Moreover, they can be produced in bacteria or yeast, making them cheaper and faster to produce than traditional antivenoms.
Another promising approach is the use of computational biology to predict the structure of venom toxins and design synthetic antibodies to neutralize them. This approach could potentially allow for the rapid development of antivenoms in response to new or evolving venom threats. However, these technologies are still in the early stages of development and require further testing and validation.
Scientific and Technical Challenges

Despite the promising progress, the development of a universal antivenom is not without its challenges. The complexity of venom diversity is a significant hurdle, with over 3,000 snake species producing varied toxin profiles that a single antivenom must target. There are also potential side effects and efficacy gaps to consider, such as incomplete neutralization for rare or hybrid venoms.
Regulatory hurdles also pose challenges. The approval of a new antivenom requires extensive human trials in diverse populations, a process that can be time-consuming and costly. Despite these obstacles, the potential benefits of a universal antivenom make it a worthwhile pursuit.
Another scientific challenge is the potential for venom resistance. Just as bacteria can develop resistance to antibiotics, there is a risk that snakes could evolve venom that is resistant to the universal antivenom. This would require ongoing monitoring and potentially frequent updates to the antivenom’s composition.
From a technical perspective, the production of a universal antivenom would require significant infrastructure and expertise. This includes facilities for the production of synthetic antibodies or nanobodies, as well as the ability to conduct rigorous testing and quality control. These requirements could pose challenges for low-income countries, which may lack the necessary resources and infrastructure.
Implementation and Accessibility Issues

Even with a successful universal antivenom, logistical barriers to deployment remain. These include cold-chain requirements and the need for training healthcare workers in remote areas. Economic factors also come into play, with the need to scale production to make the antivenom affordable for low-income countries.
Integration with existing health systems is another critical consideration. This includes aligning with WHO guidelines and forming partnerships with NGOs for distribution. Ensuring the antivenom reaches those who need it most will be a crucial aspect of its implementation.
Another potential barrier to implementation is cultural beliefs and practices. In many regions where snakebites are common, traditional healers are often the first point of contact for snakebite victims. These healers may not be familiar with the use of antivenoms, or may have cultural or religious beliefs that discourage their use. Overcoming these barriers will require education and engagement with local communities.
Accessibility issues also extend to the urban-rural divide. While urban areas may have better access to healthcare facilities and antivenoms, rural areas often face significant barriers. These include long travel distances to healthcare facilities, poor road conditions, and a lack of transportation. Addressing these issues will be crucial to ensuring the universal antivenom reaches those who need it most.
Potential Life-Saving Impact

The potential impact of a universal antivenom is significant. Scenarios project that it could reduce mortality by 50% or more in high-burden regions through broader applicability. Case studies and models show potential benefits for underserved communities, such as farmers in India or herders in Africa.
However, ethical considerations must also be taken into account. Ensuring equitable global access to the antivenom, rather than a profit-driven development by pharmaceutical companies, will be crucial to its success.
Aside from reducing mortality, a universal antivenom could also significantly reduce morbidity from snakebites. Many survivors of snakebites suffer from long-term complications such as tissue damage, amputations, and psychological trauma. By providing a more effective treatment, the universal antivenom could potentially prevent these complications, improving the quality of life for snakebite survivors.
Moreover, the development of a universal antivenom could have broader implications for global health. It could serve as a model for the development of other universal treatments, such as antivenoms for scorpion or spider bites. This could potentially save even more lives and reduce the burden of venomous bites and stings worldwide.
Future Directions and Uncertainties
Looking ahead, the next steps in research include phase II/III clinical trials and long-term monitoring for resistance or new venom variants. The broader implications for antivenom technology are also being explored, potentially extending to other toxins like scorpion or spider venoms.
While there is optimism for the availability of a universal antivenom within the next decade, real-world adoption challenges temper this. The journey towards a universal antivenom is a complex one, but the potential to save lives makes it a journey worth undertaking.
One potential future direction is the development of antivenoms that can neutralize the venom of multiple species. This would not be a truly universal antivenom, but it could provide a more flexible and cost-effective solution than the current species-specific antivenoms. However, this approach would still require the identification of the biting snake, which can be challenging in field conditions.
Another uncertainty is the potential impact of climate change on snake populations and venom composition. Changes in temperature and precipitation could affect snake habitats and behavior, potentially leading to changes in venom composition. This could pose additional challenges for the development and effectiveness of a universal antivenom.
Despite these uncertainties, the potential benefits of a universal antivenom make it a compelling area of research. With continued investment and collaboration, it is hoped that a universal antivenom can be developed that will save lives and reduce the burden of snakebites worldwide.
Source: Live Science