A groundbreaking global study involving over 1.5 million participants from 112 countries has revealed that 99% of heart attacks and strokes are linked to just four modifiable risk factors. Conducted by researchers at McMaster University and published in the Journal of the American College of Cardiology, the study underscores the potential for significant reductions in cardiovascular disease through targeted lifestyle and medical interventions. The findings also extend to heart failure, indicating that nearly all such events have identifiable cardiovascular risk factors present beforehand.
The Study’s Methodology and Global Reach
The Prospective Urban Rural Epidemiology (PURE) study forms the backbone of this research, tracking 118,105 participants from 21 countries over a decade, starting in 2003. This extensive dataset allowed researchers to collect comprehensive information on risk factors and cardiovascular outcomes, establishing causal links between them. The study’s design was meticulous, employing advanced statistical models to attribute 99% of cardiovascular events to the four primary risk factors, while adjusting for confounders like age and sex across the global dataset. This rigorous approach ensures the reliability of the findings, which have significant implications for global health policy.
By including diverse populations from high-income, middle-income, and low-income regions such as Canada, India, and rural China, the study ensures its findings are applicable beyond Western contexts. This broad inclusion is crucial for understanding how these risk factors manifest across different socioeconomic and cultural backgrounds. The study’s global reach highlights the universal nature of these risk factors, suggesting that interventions targeting them could have widespread benefits.
Identifying the Four Primary Risk Factors

High blood pressure emerged as the leading risk factor, responsible for 58% of the attributable risk in the study. Systolic blood pressure levels above 140 mmHg were found to significantly elevate the odds of heart attacks and strokes. This finding emphasizes the importance of regular blood pressure monitoring and management as a critical component of cardiovascular disease prevention.
Smoking, accounting for 22% of the risk, includes both active smoking and secondhand exposure. The PURE cohort measured smoking exposure via self-reported pack-years, highlighting the pervasive impact of tobacco use on cardiovascular health. This underscores the need for robust anti-smoking campaigns and policies to reduce smoking prevalence and its associated health risks.
Diabetes and abdominal obesity round out the list of primary risk factors, contributing 12% and 9% of the risk, respectively. These factors were assessed using fasting glucose tests and body measurements from participants. The study’s findings suggest that addressing these metabolic conditions through lifestyle changes and medical interventions could significantly reduce the burden of cardiovascular disease globally.
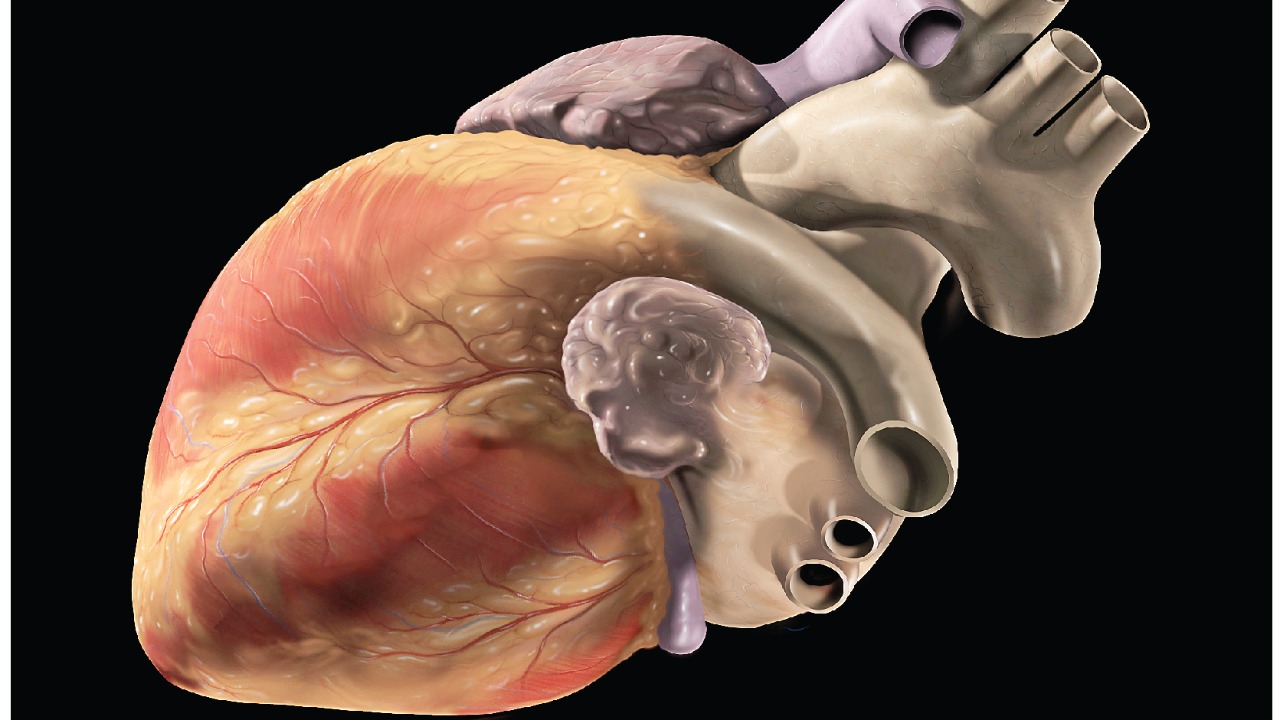
Implications for Heart Attacks, Strokes, and Heart Failure

The study’s findings have profound implications for understanding and preventing ischemic heart disease, with the four risk factors explaining 99% of cases. Notably, 80% of victims had at least two risk factors present before experiencing a cardiovascular event. This highlights the importance of comprehensive risk assessments in clinical settings to identify individuals at high risk and implement preventive measures.
In terms of stroke attribution, hypertension alone drives over 60% of cases in the dataset. The combined influence of the four risk factors predicts 99% of both hemorrhagic and ischemic stroke subtypes. This underscores the critical role of blood pressure management in stroke prevention and the need for integrated care approaches that address multiple risk factors simultaneously.
Heart failure is similarly linked to these risk factors, with 99% of incidents showing prior exposure. Obesity, in particular, exacerbates outcomes in 30% of cases from low-income settings, highlighting the intersection of socioeconomic factors and health outcomes. This finding points to the need for tailored interventions that consider the unique challenges faced by different populations.
Broader Risks and Prevention Strategies
Beyond the primary risk factors, emerging risks such as marijuana use are gaining attention. A separate analysis of over 430,000 U.S. adults from 2016–2020 data found that daily marijuana users face a 25% higher odds of heart attack and 42% for stroke compared to non-users. This highlights the evolving landscape of cardiovascular risk factors and the need for ongoing research to understand their implications fully.
Prevention strategies are crucial for mitigating these risks. The study recommends screening for the four primary risk factors in primary care settings, with a particular emphasis on maintaining blood pressure below 120 mmHg to cut global risk by 40%. Such measures could dramatically reduce the incidence of cardiovascular events and improve population health outcomes.
Public health applications of these findings include policy initiatives such as smoking bans and diabetes management programs. If implemented effectively in middle- and low-income countries, these strategies could prevent up to 80% of cardiovascular deaths. This underscores the potential for policy-driven interventions to make a significant impact on global health.
For more detailed insights, you can read the full study on ZME Science, Economic Times, and Yahoo News. Additional perspectives on the implications for heart failure can be found on HCPLive, while emerging risks like marijuana use are discussed in detail on CNN.