Cancer is killing far fewer people in early and mid‑adulthood than it did a generation ago, a public‑health success story built on better screening, treatment, and prevention. Yet inside that good‑news trend sits a stark exception: colorectal tumors are striking younger adults more often and claiming more lives, even as other malignancies retreat.
I see a split narrative emerging. On one side, overall cancer mortality in people under 50 has nearly halved, with deaths dropping by roughly 44% since the 1990s. On the other, colon and rectal cancers have climbed into the top spot as the leading cause of cancer death in this age group, reshaping how doctors, patients, and policymakers think about risk in what used to be considered the “low‑concern” decades.
Overall cancer deaths are falling fast in people under 50
For younger adults, the broad picture is encouraging. Analyses of national data show that cancer deaths among people under 50 have nearly halved, reflecting major gains in early detection and treatment across multiple tumor types. One report found that Cancer deaths of have dropped sharply, with improvements in breast, lung, and blood cancers driving much of the decline. These gains are not abstract statistics; they translate into parents living to see their children grow up and workers staying in the labor force instead of exiting early because of illness.
Researchers tracking these trends have quantified the shift even more precisely. One analysis reported that Overall cancer deaths among people under 50 have fallen by 44% since the 1990s, a drop attributed to better screening programs, more effective therapies, and reductions in some key risk factors like smoking. I read that as proof that long‑term investments in cancer control can pay off, even if the benefits are uneven across different types of disease.
Colorectal cancer has surged into the top killer for younger adults
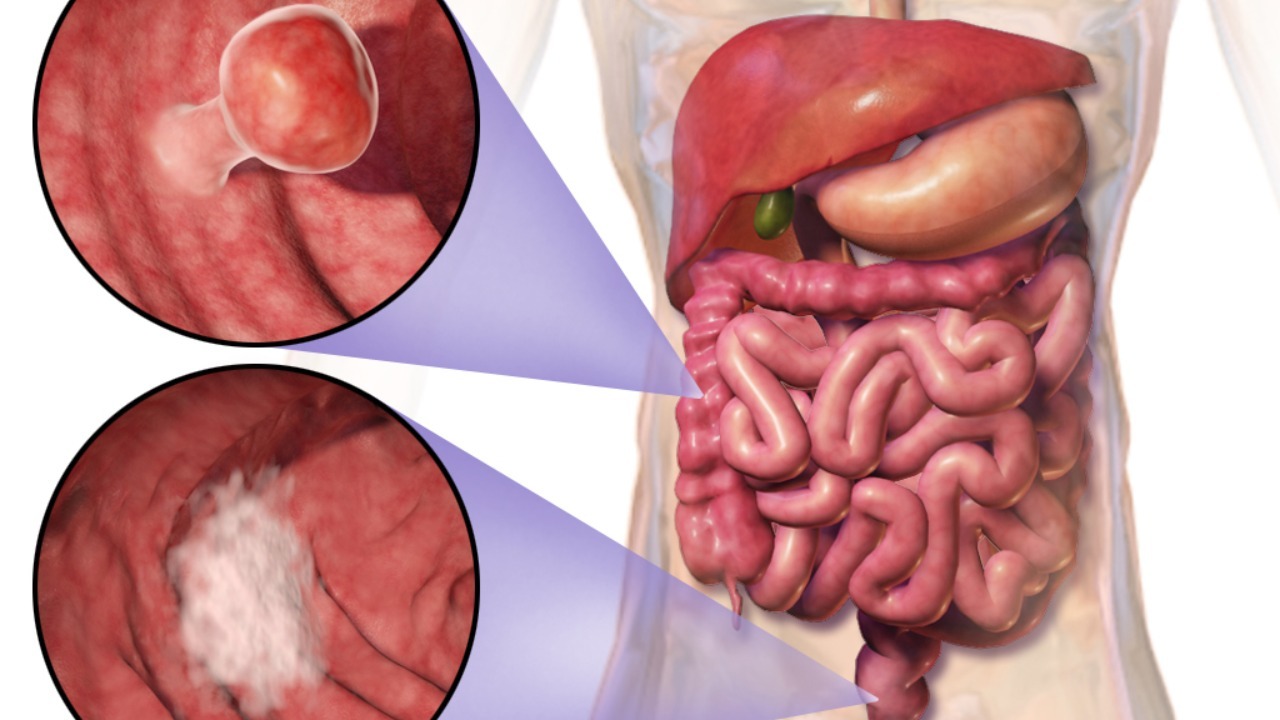
Against that backdrop of progress, colorectal cancer has moved in the opposite direction. A JAMA Study found that colorectal cancer is now the leading form of cancer deaths in people under 50, after ranking fifth from 1990 to 1994. That shift means tumors in the colon and rectum have leapfrogged more familiar threats like breast and lung cancer in this age group, a reversal that would have seemed unlikely a generation ago.
Multiple analyses converge on the same alarming conclusion. A new study by American Cancer Society researchers reported that colorectal cancer is now the top cause of cancer mortality in patients under 50 years, even as overall cancer deaths in that group fall. Another report underscored that colon cancer is now the No. 1 cause of cancer deaths in Americans under 50, and that this grim milestone arrived years earlier than experts had projected. I see that as a clear signal that the old assumption of colorectal cancer as a disease of retirement age no longer holds.
Why early‑onset colorectal cancer is rising while others fall
Scientists are still piecing together why colorectal tumors are climbing in younger adults while other cancers decline. One analysis noted that, since the mid‑1990s, there has been a steady increase in early‑onset cases, with roughly one in five people diagnosed with colorectal cancer now under 55, a pattern highlighted in a report on CRC trends. I read that as evidence of a genuine shift in disease biology and exposure, not just better detection.
Researchers like Cao, who is leading a first‑of‑its‑kind program called PROSPECT, are probing how environment, lifestyle, and genetics intersect to drive this rise in early‑onset cancer. More than a few studies point to a so‑called birth cohort effect, suggesting that people born in more recent decades may carry higher risk because of exposures that began in childhood. I see this as a warning that the roots of today’s colorectal cancers may lie in long‑running changes in diet, antibiotic use, and sedentary behavior that started years before symptoms appear.
Gut health, lifestyle, and other suspected drivers
When I look at the emerging evidence, the gut itself appears to be a central player. Experts have highlighted that people with colorectal cancer often have less variety in their Gut microbiome, and that certain bacterial patterns may promote inflammation and tumor growth. A detailed overview of early‑onset colon cancer from a major clinic noted that Gut microbiome changes, heavy antibiotic use early in life, highly processed diets, obesity, and sedentary behavior in youth all appear to raise risk. None of these factors alone explains the surge, but together they sketch a picture of a digestive system under chronic stress from an early age.
Other researchers emphasize that the pattern is likely multifactorial rather than driven by a single culprit. One analysis reported that Researchers have cited several reasons colorectal cancer could be rising in younger people, and that incidence has been increasing by about 1.1% per year since 2005. Another report from a major academic Cancer Center quoted Christopher Lieu, a leader at that center, stressing that the new data from the Cancer Center and the American Cancer Society point to an urgent need to understand and reverse this trend. I interpret that as a call for deeper research into how modern living is reshaping cancer risk long before midlife.
Screening, awareness, and what needs to change
If colorectal cancer is rising in younger adults, the most immediate lever is earlier and broader screening. The American Cancer Society has already lowered its recommended starting age for average‑risk colorectal screening from 50 to 45, a shift reflected in its ACS recommendations. I see that change as a direct response to the data, an acknowledgment that waiting until 50 misses too many cancers that are already advanced by the time they are found.
Clinicians on the front lines are echoing that urgency. One interview with Dr. Corley, a specialist focused on Colon cancer, emphasized that tumors are becoming more common in people under 50 and that Lowering the recommended screening age is one of the few tools available right now. Dr. Corley underscored that the most powerful thing we have is screening, because it can catch precancerous polyps before they turn deadly. I read that as a reminder that technology already exists to blunt this trend if people and health systems actually use it.
There is also growing recognition that awareness and access gaps are holding back progress. A study of people aged 40 and older visiting primary care clinics in Al‑Khobar, in Saudi Arabia’s Eastern Province, found limited knowledge of colorectal cancer and significant barriers to getting tested. The authors concluded that this trend underlines the fact that it is crucial to direct efforts toward early detection to lower incidence and mortality, and they noted the importance of policies that support screening from 50 years old. I see parallels in the United States, where insurance coverage, primary care access, and cultural discomfort with colonoscopy can all delay lifesaving tests.
More from Morning Overview