Ancient viral fossils buried in our DNA are offering fresh clues about how today’s respiratory pathogens infect and spread. By tracing the shared architecture between long-extinct retroviruses and modern viruses that target the lungs, I can map a story that runs from deep evolutionary time to the hospital ward.
What emerges is not a simple tale of one virus turning into another, but a structural playbook that keeps getting reused. The same tricks that let retroviruses slip into host cells and co-opt genetic machinery now echo in the way contemporary respiratory viruses attach, fuse and replicate.
How retroviruses work, in structure not just in name
To understand why ancient retroviral blueprints matter for respiratory disease, I first need to be precise about what a retrovirus is. Retroviruses are enveloped RNA viruses that carry the enzyme reverse transcriptase, package their genome in a capsid, and integrate a DNA copy into the host chromosome as a provirus, a life cycle that distinguishes them from other RNA viruses that never enter the genome in this way. That core definition, which includes hallmark genes like gag, pol and env, is laid out in reference descriptions of the retrovirus family and underpins how virologists classify these pathogens.
Once inside a cell, the retroviral particle uncoats, reverse transcriptase copies its RNA into DNA, and integrase inserts that DNA into host chromosomes, turning the infected cell into a factory for new virions. Educational breakdowns of this process emphasize how the env gene encodes surface glycoproteins that bind receptors, while gag and pol build the internal structure and enzymatic toolkit that make this integration possible, a division of labor that is central to the way retroviruses replicate and persist.
Endogenous retroviruses, the viral fossils in our genome
Over evolutionary time, some retroviruses infected germline cells and became permanent fixtures in the genome, passed from parent to offspring as endogenous retroviruses rather than as active infections. Surveys of the human genome show that these sequences, often called ERVs, now account for a substantial fraction of our DNA, with many copies degraded by mutation but still recognizable as ancient viral remnants, a pattern documented in detailed analyses of endogenous retroviruses and their distribution across chromosomes.
Most of these viral fossils are no longer capable of producing infectious particles, yet some retain open reading frames or regulatory elements that can be co-opted by the host. Researchers have shown that certain ERV-derived envelope proteins have been repurposed for key physiological roles, including cell fusion events in the placenta, while other loci can influence nearby gene expression, illustrating how the structural and regulatory motifs of ancient retroviruses have been woven into normal human biology rather than simply silenced as genomic junk.
What ancient capsids reveal about viral architecture
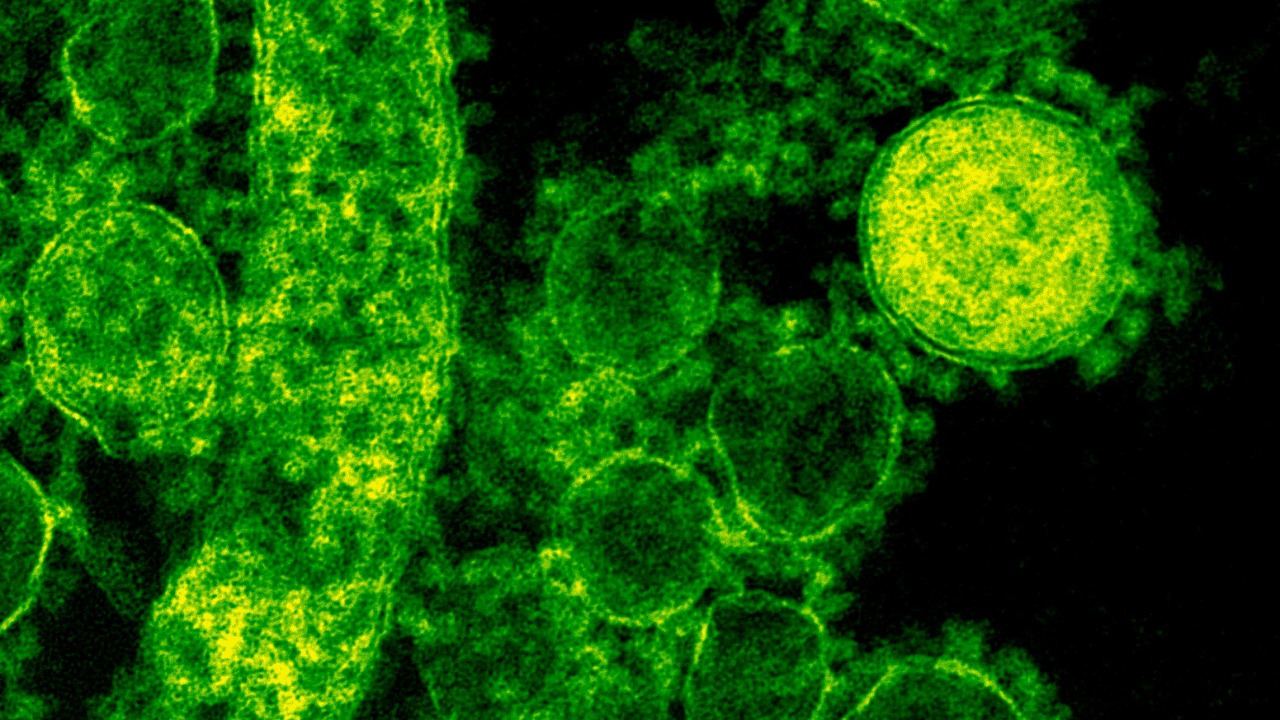
The structural core of retroviruses, particularly the capsid that surrounds the RNA genome, has been dissected in high resolution to understand how these particles assemble and disassemble. Classic work on retroviral capsid proteins used biochemical and structural approaches to map how individual subunits interact, revealing conserved domains that control lattice formation, curvature and stability, insights that are captured in foundational studies of retroviral capsid structure and its role in the viral life cycle.
Those same capsid features determine how the virus traffics through the cytoplasm, docks at nuclear pores and times uncoating, which in turn shapes how efficiently the genome can integrate. More recent structural virology has extended this logic to compare capsid and envelope architectures across viral families, showing that certain folds and assembly strategies recur even when the viruses are not closely related, a convergence that becomes clear in comparative analyses of viral protein structure and the constraints that govern particle design.
Echoes of retroviral design in respiratory pathogens
Modern respiratory viruses, including those that are not classified as retroviruses, still rely on a familiar set of structural maneuvers to infect airway cells. They must attach to receptors on epithelial surfaces, trigger membrane fusion or endocytosis, and then uncoat in a controlled way so their genomes can access replication machinery, a sequence of events that mirrors the entry and fusion steps refined by retroviral env proteins even if the downstream replication strategy differs. Comparative overviews of viral families highlight how these shared requirements have driven similar solutions in envelope glycoprotein design and fusion mechanisms, themes that are emphasized in structural surveys of enveloped respiratory viruses and their entry pathways.
In practical terms, that means the same kinds of heptad repeat regions, fusion peptides and receptor binding domains that define retroviral envelopes also appear in the spike or fusion proteins of respiratory pathogens that target the lungs. Educational explainers on viral entry show how these motifs undergo large conformational changes to bring viral and cellular membranes together, a choreography that can be visualized in stepwise animations of viral fusion and then mapped back onto the static structures solved by cryo-electron microscopy and X‑ray crystallography.
From viral fossils to immune responses in the lung
The presence of endogenous retroviral sequences in our genome is not just an evolutionary curiosity, it also shapes how the immune system responds to infection in tissues like the lung. Some ERV-derived elements can be transcribed and translated under certain conditions, producing RNA or protein fragments that innate sensors recognize, effectively priming pattern recognition pathways that also respond to active respiratory viruses. Reviews of host–virus interactions describe how these endogenous signals can tune interferon responses and other antiviral defenses, a relationship that becomes evident in analyses of innate immune sensing and the molecular triggers that activate it.
At the same time, the immune system must avoid overreacting to every trace of viral ancestry embedded in the genome, particularly in barrier tissues that are constantly exposed to environmental antigens. Studies of mucosal immunity in the respiratory tract show how regulatory networks balance tolerance and defense, and some of those networks appear to have been shaped by long-term exposure to ERV-derived products, a coevolutionary process that is discussed in depth in work on immune regulation and the fine line between protective inflammation and damaging autoimmunity.
Structural insights feeding into vaccine and drug design
Because the structural motifs that retroviruses pioneered are reused across respiratory pathogens, they have become prime targets for vaccines and antiviral drugs. Neutralizing antibodies often recognize conserved regions of envelope or fusion proteins that are constrained by their role in receptor binding or membrane merger, and structural vaccinology efforts now routinely map these epitopes at atomic resolution to guide immunogen design, an approach that builds directly on decades of work dissecting viral protein conformation and the way antibodies lock them into nonfunctional states.
Small-molecule antivirals also exploit structural vulnerabilities, from pockets in polymerases to interfaces between capsid subunits that are essential for assembly. Detailed structural and functional studies of viral enzymes and scaffolds have identified such druggable sites, and some of those efforts explicitly compare retroviral and respiratory virus proteins to find shared features that could support broad-spectrum inhibitors, a strategy outlined in technical reports on antiviral target discovery and the search for conserved structural motifs.
Why the deep past matters for the next outbreak
Looking across these threads, the connection between ancient retroviral architecture and modern respiratory disease is less about direct ancestry and more about a recurring engineering solution to the problem of entering and exploiting host cells. The same capsid geometries, envelope fusion strategies and genome integration or replication tricks that once allowed retroviruses to colonize germlines now inform how we interpret the behavior of new pathogens that emerge in the airways. Synthesizing insights from structural biology, genomics and immunology, researchers are increasingly treating ERVs and retroviral fossils as a reference library for decoding the vulnerabilities of contemporary respiratory viruses, a perspective that is reinforced in broad surveys of virus evolution and the constraints that shape their form.
For public health, that means the next generation of diagnostics, vaccines and therapeutics will likely lean even more heavily on this deep-time perspective. By recognizing that the molecular tricks used by a virus in the lungs today echo designs that have been circulating in genomes for millions of years, I can better anticipate which structural features are most likely to persist, which are most exposed to immune pressure, and where interventions will have the greatest leverage, a strategy that aligns with ongoing efforts to map conserved viral structures and translate them into durable tools against respiratory disease.
More from MorningOverview