Researchers have made a groundbreaking advancement in the field of regenerative medicine with the development of a miniature 3D printer, equipped with a lens the size of a grain of salt. This innovative device has the potential to construct living tissue directly inside the human body, reducing the need for invasive surgeries and paving the way for on-site tissue regeneration using biocompatible materials and precise laser-based printing techniques. The technology, which has already demonstrated its feasibility in preclinical models, marks a significant step towards personalized medicine.
The Core Innovation: Salt-Grain-Sized Lens Technology

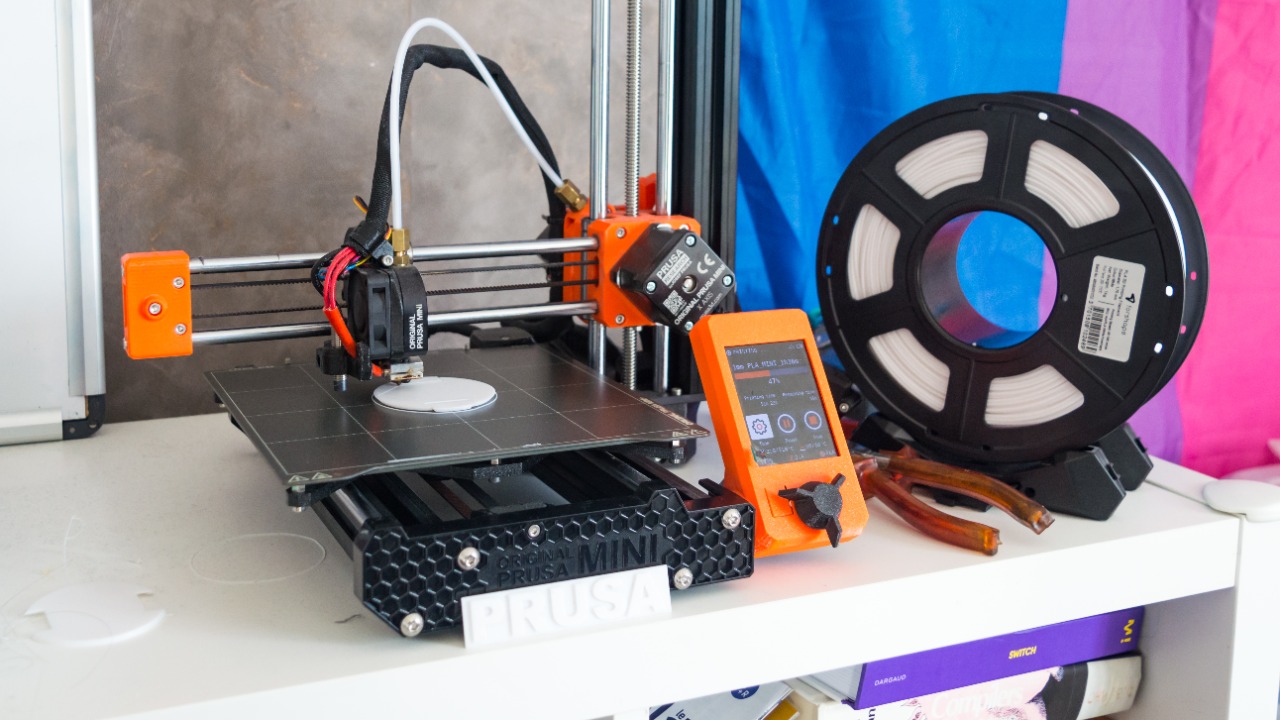
The microscale design of the lens is a key feature of this innovative technology. It enables high-resolution bioprinting at the cellular level without the need for large equipment, making it possible to implant the device via minimally invasive procedures. The lens works by focusing laser beams to deposit bio-inks layer by layer, forming functional tissue structures comparable in size to a grain of salt for targeted internal applications. This level of precision is crucial for the successful integration of the printed tissue with the body’s existing structures (Interesting Engineering).
Another important aspect of the lens technology is its biocompatibility. The material used for the lens is designed to integrate safely within the body without triggering immune responses during tissue construction. This ensures that the process of bioprinting can take place without causing harm or discomfort to the patient (Rude Baguette).
Mechanism of In-Body Tissue Construction

The mini 3D printer is delivered into the body either endoscopically or via injection. Once inside, it is activated upon a trigger signal to begin the process of printing vascularized tissue scaffolds. This process involves the use of patient-specific stem cells in the bio-ink formulation, which the printer assembles into organ-like structures to repair damage from injuries or diseases (Interesting Engineering).
The device is also equipped with wireless controls for real-time adjustments, ensuring precise alignment with the body’s native tissues. This level of control is crucial for the successful integration of the printed tissue with the body’s existing structures (Rude Baguette).
Potential Applications in Regenerative Medicine
One of the most promising applications of this technology is in the field of cardiology. For patients who have suffered a myocardial infarction, the printer could be used to rebuild damaged heart tissue directly in situ. This could significantly improve recovery outcomes and reduce the need for invasive surgical procedures (Interesting Engineering).
The technology also has potential applications in neurology. For example, it could be used to print neural scaffolds to bridge spinal cord injuries and restore function without the need for open surgery. Additionally, the technology could be used for cartilage regeneration in joints, potentially reducing recovery times for arthritis patients through localized bioprinting (Rude Baguette).
Advantages Over Traditional Surgical Methods
Compared to traditional tissue engineering methods, which often require tissue harvesting and lab-culturing before transplantation, the mini 3D printer offers a more efficient and less invasive solution. By operating autonomously inside the body, the device reduces surgical risks, including lower infection rates and shorter hospital stays (Interesting Engineering).
Furthermore, by eliminating the need for multiple procedures, the technology can also offer cost efficiencies. This could make advanced tissue repair more accessible, extending its benefits beyond specialized centers (Rude Baguette).
Challenges and Safety Considerations

Despite its promising potential, the technology also faces several challenges. One technical hurdle is ensuring the long-term degradation of the printer without leaving any residue in the body, which requires advanced biomaterials testing (Interesting Engineering).
Regulatory pathways also present a challenge. Before the technology can be used in human trials, it will need to gain FDA approval to validate tissue viability and integration. There are also ethical concerns around in vivo printing accuracy to prevent the creation of malformed tissues or unintended growth (Rude Baguette).
Future Developments and Research Directions

Looking ahead, the technology could be scaled up to print larger organs such as kidneys by combining multiple mini printers in a networked system. This would represent a major breakthrough in the field of organ transplantation (Interesting Engineering).
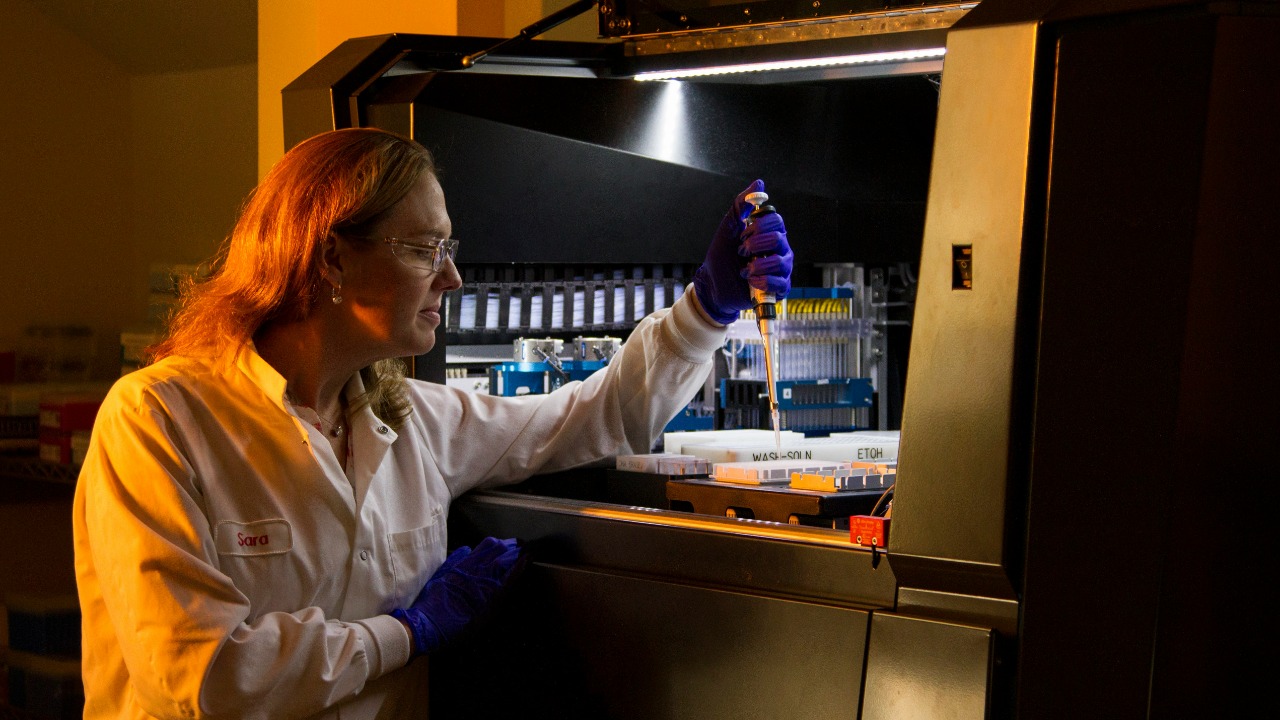
Research is also ongoing to refine the resolution and bio-ink compositions for diverse tissue types. This involves interdisciplinary collaborations between engineers and biologists. Preclinical studies demonstrating successful tissue functionality in animal models are paving the way for clinical translation, bringing us one step closer to a future where personalized medicine is the norm (Rude Baguette).