Researchers have made a significant breakthrough in the field of pain management by identifying a specific brain circuit that can effectively switch off chronic pain signals.1 This discovery builds on earlier findings from 2019 at Stanford University, where scientists pinpointed brain cells responsible for the unpleasant emotional aspect of pain.5 The recent discovery, reported in October 2025, links pain modulation to circuits also involved in hunger and fear responses, potentially revolutionizing pain management for millions affected by chronic conditions.3
The Science Behind the Brain Circuit

The brainstem plays a crucial role in integrating pain signals with other survival responses like hunger and fear. The identified circuit in the brainstem, when activated, suppresses chronic pain without affecting acute pain perception.3 This circuit involves a specific neural pathway, including neurons that, when stimulated, interrupt pain transmission to higher brain areas responsible for perception.1
Experimental evidence from animal models shows immediate pain relief upon circuit activation, with no reported side effects on motor function. This suggests that the circuit could be a viable target for non-invasive pain relief techniques.2
Mechanisms of Pain Switching

The circuit uses inhibitory signals to “gate” chronic pain, a mechanism similar to natural pain modulation during states of high arousal like fear.3 Neurotransmitters play a significant role in the switch-off process, as revealed by imaging and stimulation studies conducted in 2025.1
This mechanism specifically targets chronic rather than acute pain. This specificity is evident in examples from prolonged injury models in research, where chronic pain persists due to altered neural patterns in the cortex.2 This distinction between chronic and acute pain is crucial in developing targeted treatments for chronic pain conditions.
Historical Context and Prior Discoveries

Research on brain signals for chronic pain has been ongoing for several years. In 2023, researchers found that pain persists due to altered neural patterns in the cortex.4 This discovery provided a foundation for understanding the neural basis of chronic pain.
In 2019, a Stanford study identified “aversion neurons” in the brain that amplify the emotional distress of pain, setting the stage for circuit-based interventions.5 The 2025 discovery builds on this work, linking the control of pain unpleasantness to specific circuits in the brainstem.1
Potential Therapeutic Applications

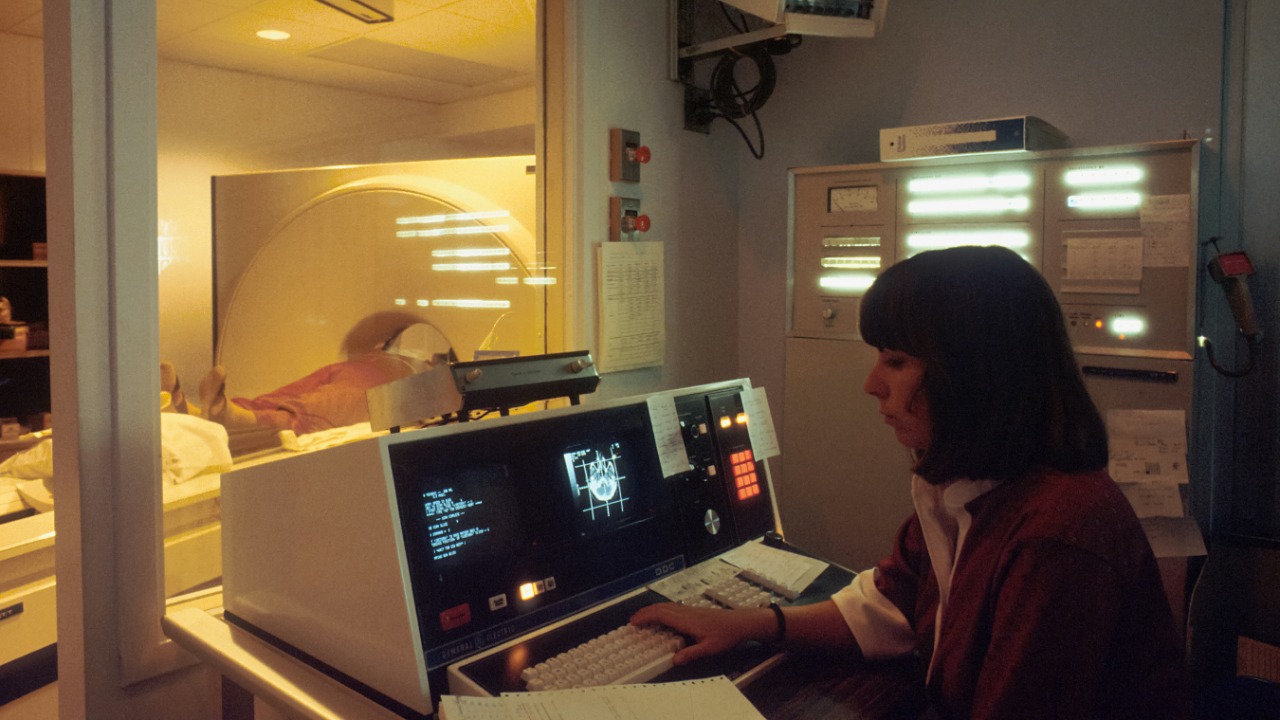
The discovery of this brain circuit opens up potential new avenues for non-opioid treatments. Non-invasive techniques like targeted neuromodulation could be used to activate the circuit, potentially reducing reliance on opioids for chronic pain sufferers.2
There are promising prospects for clinical trials, including human applications for conditions like neuropathy, based on the circuit’s specificity to chronic pain.1 Existing therapies could be integrated with circuit stimulation, such as combining it with cognitive behavioral approaches to enhance pain relief.4
Challenges and Future Research Directions

While the discovery is promising, there are limitations in translating animal findings to humans, including variability in brainstem responses across individuals.3 Ethical considerations for neuromodulation devices also need to be explored, drawing from past pain research safety profiles since 2019.5
Future research directions could include longitudinal studies on circuit durability in treating long-term chronic pain, starting from 2025 data.1 This would provide valuable insights into the long-term effectiveness of circuit-based interventions for chronic pain.
Broader Implications for Neuroscience
The discovery reframes pain as part of a unified brainstem network handling fear and hunger, impacting models of emotional processing.3 This could have ripple effects on related disorders, like anxiety-linked pain amplification identified in 2023 brain signal studies.4
Interdisciplinary advancements, such as AI-assisted mapping of similar circuits for other sensory modulations, could be spurred by this discovery.2 The identification of this brain circuit marks a significant step forward in our understanding of pain and offers hope for more effective treatments for chronic pain in the future.