
Transcranial Magnetic Stimulation (TMS) is a non-invasive procedure that uses magnetic fields to stimulate nerve cells in the brain. This treatment, often used for depression, can temporarily interrupt brain activity, leading to a variety of effects. It is crucial to understand the mechanisms, applications, and implications of this intriguing technology to appreciate its potential impact on mental health care.
The Science Behind Transcranial Magnetic Stimulation

Mechanism of Action
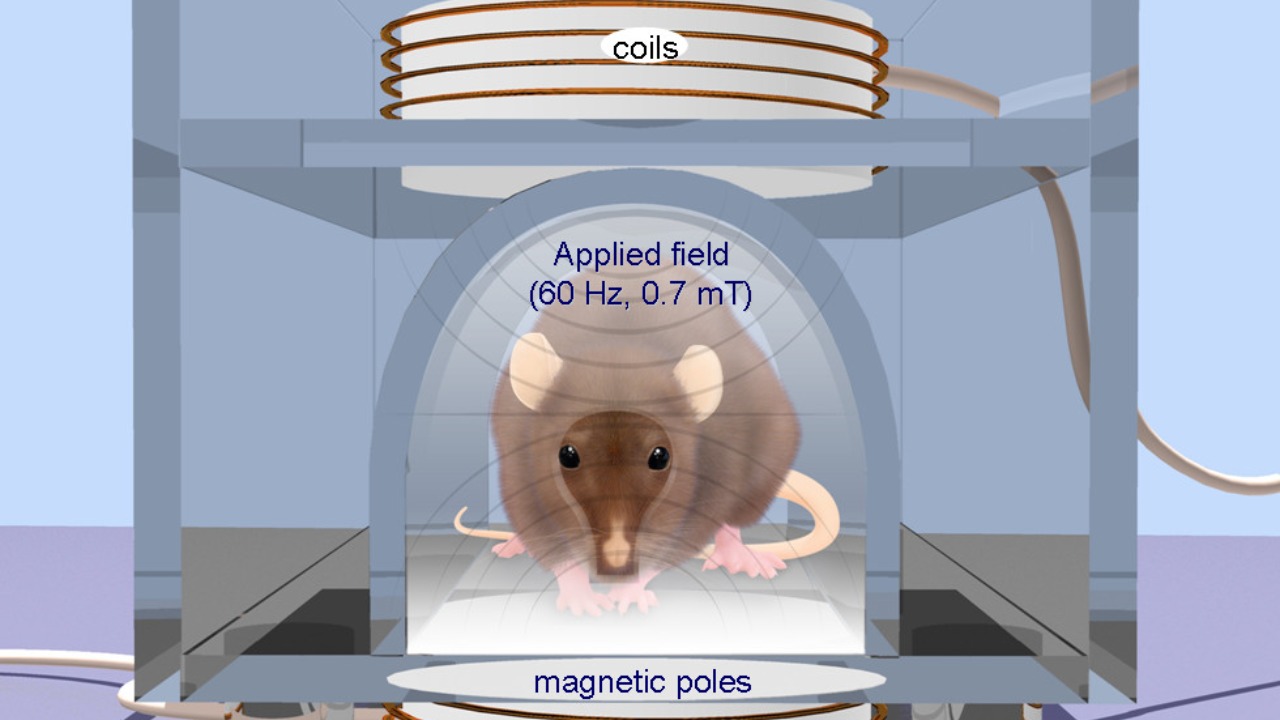
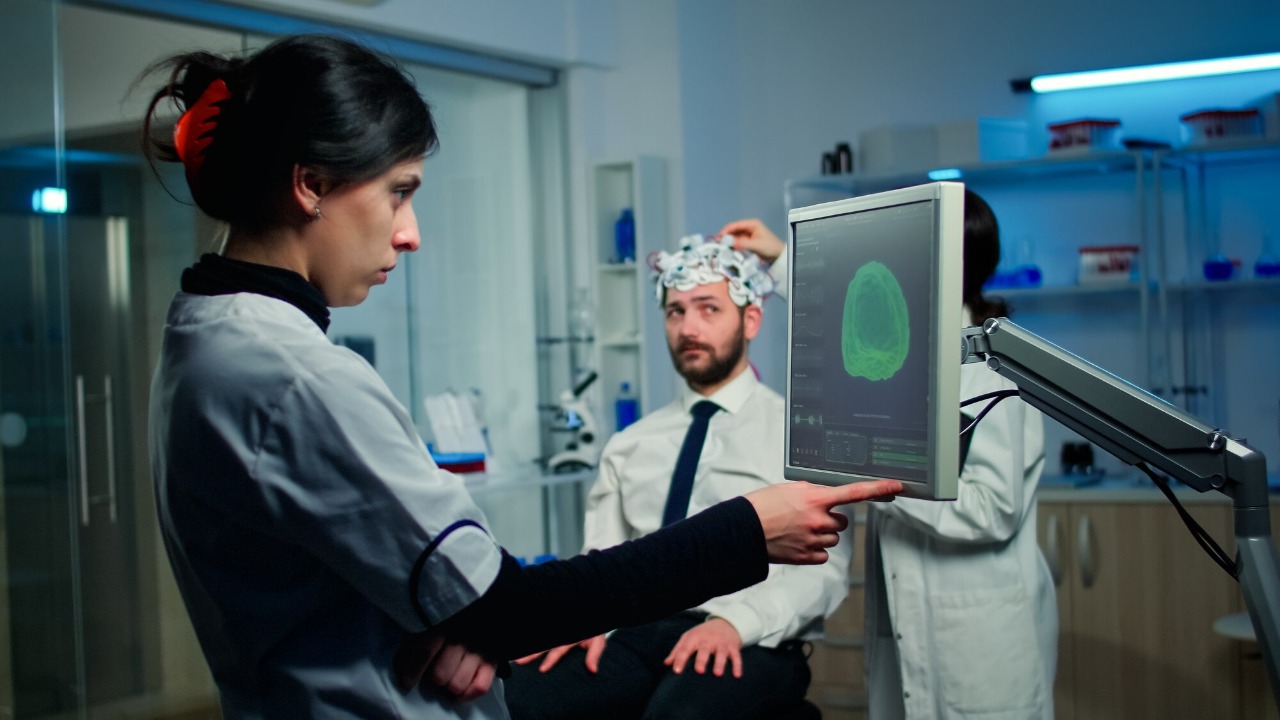
TMS operates on the principle of electromagnetic induction, a concept first proposed by Michael Faraday. In TMS, a coil placed near the scalp emits a magnetic pulse that induces an electric current in the brain. This current can modulate neuronal activity, either enhancing or suppressing brain function in targeted areas. Through this method, TMS can affect the brain’s electrical circuits without the need for surgical intervention, making it a less invasive option for altering brain activity.
The ability of TMS to modulate neuronal circuits allows it to influence brain functions, such as mood regulation and cognitive processes. By delivering repeated pulses, TMS can induce long-lasting changes in synaptic plasticity, which is the brain’s ability to strengthen or weaken synapses over time. This modulation of synaptic connections is believed to underlie the therapeutic effects of TMS in various psychiatric and neurological disorders.
Target Areas and Frequencies
TMS is commonly applied to the prefrontal cortex, a brain region associated with mood regulation and executive function. The targeting of specific brain areas is crucial because different regions are responsible for various cognitive and emotional processes. The exact location and depth of stimulation are determined using neuroimaging techniques, ensuring precise delivery of magnetic pulses to the intended site.
The frequency and intensity of magnetic pulses are critical factors in achieving the desired therapeutic outcome. Low-frequency TMS, typically around 1 Hz, is used to decrease neuronal excitability, while high-frequency TMS, ranging from 5 to 20 Hz, is used to increase excitability. The choice of frequency depends on the condition being treated, as well as the specific goals of the therapy. Personalized TMS protocols are being developed to optimize treatment efficacy and minimize side effects.
Clinical Applications of TMS
Treatment of Depression
TMS has gained recognition as a FDA-approved therapy for treatment-resistant depression. Patients who do not respond to conventional antidepressant medications may benefit from TMS, which offers a non-pharmacological alternative. Clinical studies have shown that TMS can significantly reduce depressive symptoms and improve quality of life for many patients.
The success rates of TMS in treating depression vary, with some studies reporting response rates of up to 60%. Patient experiences can differ based on individual factors, such as the severity of depression and previous treatment history. Despite its efficacy, TMS is not a cure-all; ongoing therapy may be necessary to maintain benefits, and some patients may require adjunctive treatments to achieve optimal outcomes.
Emerging Uses
Beyond depression, TMS is being explored as a treatment for a wide range of psychiatric and neurological conditions. Preliminary research suggests that TMS may help alleviate symptoms of anxiety, PTSD, and schizophrenia by modulating dysfunctional brain circuits. These emerging applications hold promise but require further investigation through rigorous clinical trials to establish their efficacy and safety.
Current research is also examining the potential of TMS in addressing neurocognitive disorders, such as Alzheimer’s disease and chronic pain conditions. By expanding the scope of TMS applications, researchers hope to provide new therapeutic options for patients who have limited treatment choices. The versatility of TMS makes it a valuable tool in the ongoing quest to understand and treat complex brain disorders.
Potential Risks and Side Effects
Common Side Effects
While TMS is generally considered safe, it is not without side effects. The most common side effects include mild headaches and scalp discomfort, which typically occur during or shortly after treatment. These side effects are usually transient and can be managed with over-the-counter pain relievers or adjustments to the TMS protocol.
To minimize discomfort, clinicians often start with lower intensities and gradually increase the dosage as tolerated by the patient. Regular monitoring and communication between the patient and healthcare provider are essential to ensure a positive treatment experience and address any concerns that may arise during the course of therapy.
Serious Concerns and Criticisms
Despite its relatively benign side effect profile, TMS is not without its risks. In rare cases, TMS can induce seizures, particularly in individuals with a history of epilepsy or other seizure disorders. The risk of seizures is related to the intensity and frequency of the magnetic pulses, highlighting the importance of careful patient selection and protocol customization.
Critics of TMS have raised concerns about its safety and efficacy, citing anecdotal reports of adverse outcomes. While these reports are not representative of the majority of TMS experiences, they underscore the need for ongoing research and post-market surveillance to ensure the continued safety and effectiveness of TMS as a therapeutic modality.
Ethical and Societal Considerations

Informed Consent and Patient Autonomy
Obtaining informed consent is a fundamental ethical requirement in TMS treatment. Patients must be provided with comprehensive information about the procedure, including potential risks, benefits, and alternatives. This ensures that patients can make informed decisions about their care and exercise autonomy over their treatment choices.
Challenges in achieving truly informed consent arise from the complexity of the information and the variability in individual patient understanding. Healthcare providers must strive to communicate clearly and effectively, using language that is accessible to patients from diverse backgrounds. Ensuring patient autonomy is not only an ethical obligation but also a critical component of patient-centered care.
Accessibility and Cost
The availability and affordability of TMS treatments are significant concerns for patients and providers alike. The high cost of TMS equipment and the need for specialized training can limit the number of clinics offering this treatment, creating barriers to access for patients in underserved areas. Additionally, insurance coverage for TMS varies widely, with some policies offering limited or no reimbursement for the procedure.
Socio-economic factors further complicate access to TMS, as individuals from lower-income backgrounds may struggle to afford treatment, even if insurance coverage is available. Addressing these barriers requires advocacy and policy changes to ensure that all patients have equitable access to effective mental health treatments.
The Future of TMS in Neuromodulation

Advancements in Technology
The field of TMS is rapidly evolving, with advancements in technology poised to enhance its efficacy and accessibility. Innovations in TMS equipment, such as more precise targeting and improved coil designs, are expected to optimize treatment outcomes and reduce the risk of side effects. These technological improvements will likely expand the range of conditions that TMS can effectively treat.
Personalized medicine is also playing a role in the evolution of TMS. By tailoring treatment protocols to individual patient profiles, clinicians can enhance the therapeutic effects of TMS while minimizing adverse outcomes. This approach holds the promise of more effective and patient-specific interventions, aligning with the broader trend towards precision medicine in healthcare.
Integration with Other Therapies
TMS is increasingly being integrated with other therapeutic modalities to enhance its effectiveness. Combining TMS with psychotherapy, such as cognitive-behavioral therapy (CBT), or with pharmacological treatments can provide synergistic effects, leading to more comprehensive and sustained improvements in mental health conditions.
The vision of TMS within the broader landscape of mental health care is one of integration and collaboration. By working in concert with other treatment options, TMS has the potential to offer a more holistic approach to mental health care, addressing the diverse needs of patients and improving overall outcomes. As research continues to explore these combinations, the future of TMS looks promising, with the potential to transform the way we approach and treat mental health disorders.